The 2020 Nobel Prize in Physiology or Medicine
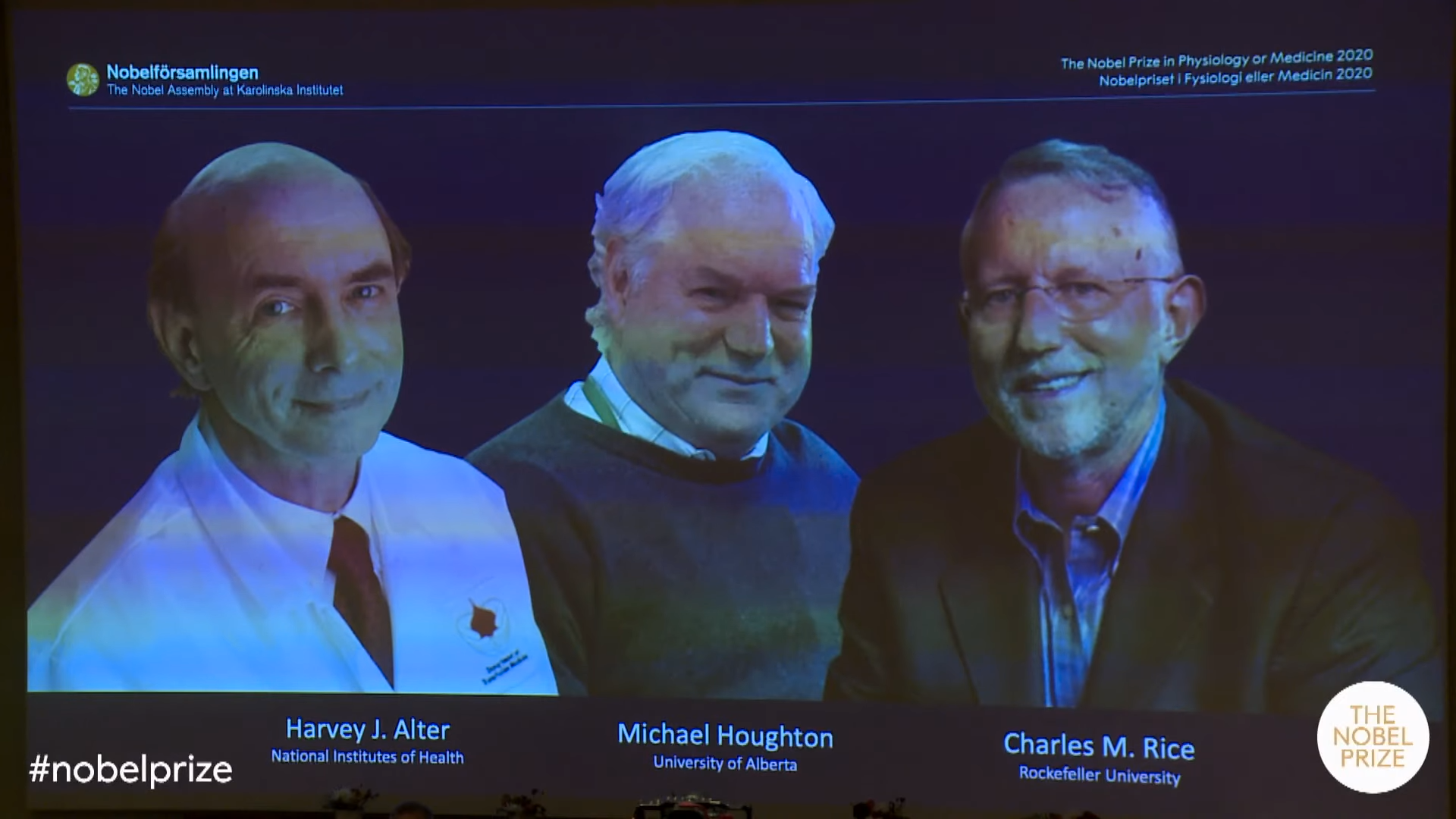
The 2020 Nobel Prize in Physiology or Medicine has been awarded jointly to Harvey J. Alter, Michael Houghton, and Charles M. Rice “for the discovery of Hepatitis C Virus.”
Harvey J. Alter is currently a Distinguished Investigator at the famed National Institutes of Health (NIH), Bethesda, USA where he has been since his career began and is the chief of the infectious disease section and the associate director for research of the Department of Transfusion Medicine at the Warren Grant Magnuson Clinical Center; Michael Houghton did his work at the biotech giant Chiron Corporation and relocated to the University of Alberta in 2010 and is currently a Canada Excellence Research Chair in Virology and the Li Ka Shing Professor of Virology at the University of Alberta where he is also Director of the Li Ka Shing Applied Virology Institute; whilst Charles Rice has been the Maurice R. and Corinne P. Greenberg Professor at Rockefeller University since 2001 but established his research group at Washington University School of Medicine, St Louis in 1986 and became full Professor in 1995.
Click here for the press release.
1. Harvey Alter
In the 1960s, a blood transfusion was a risky prospect and researchers were witnessing an alarming rise in the number of people who received blood subsequently succumbing to hepatitis, a condition that caused an inflammation of the liver. To combat this problem, Harvey Alter spearheaded a project at the National Institutes of Health (NIH) aimed at uncovering and rooting out the causes whilst reducing the risk of transfusion-associated hepatitis by testing interventions that might reduce disease transmission. A part of the puzzle was solved in 1967 when the legendary physician-scientist Baruch Blumberg pinpointed the virus hepatitis B as a cause, an important study where Alter had co-discovered the Australia antigen, a key to detecting hepatitis B virus. Just a decade later, the 1976 Nobel Prize in Physiology or Medicine was awarded jointly to Baruch S. Blumberg and D. Carleton Gajdusek “for their discoveries concerning new mechanisms for the origin and dissemination of infectious diseases.”
By measuring the concentrations of an enzyme called alanine aminotransferase (ALT) that the liver produces when inflamed, the scientists could detect early indications of disease. This key test for hepatitis revealed that the illness was striking about 30 percent of people who were receiving transfusions. This pioneering work led to the US instituting blood- and donor-screening programs that made a massive impact on the safety of the blood supply and hepatitis rates plunged to 10 percent but Alter also discovered that these efforts left a large residual pool of contaminated blood. He studied the associated disease and in collaboration with Robert Purcell and Stephen Feinstone at the NIH, and using chimpanzees as an animal model for the disease, Alter showed that not a single one of transfusion-associated non-B hepatitis cases were related to the hepatitis A virus and concluded that another culprit was triggering the majority of disease. Alter called it “non-A, non-B hepatitis” (NANBH) because it was caused by an agent other than the two hepatitis viruses known at the time.
Now the researchers wanted to pin down the troublemaking blood contaminant and using the samples that infected chimpanzees as a source for the NANBH agent, the Alter team attempted to devise a procedure that would distinguish individuals who carried the infectious material from those who didn’t. They hoped that they could concoct a simple serologic test with which to screen the blood supply, as had been done successfully for many other germs, and employed every conventional technique designed to detect harmful microbes or the body’s immune response to them but all attempts to identify proteins from the presumptive NANBH infectious agent or the host’s antibodies to such proteins failed. In the meantime, both the Alter-Purcell team at NIH and Daniel Bradley’s group at the Centers for Disease Control (CDC) were characterizing the agent. By filtering blood through different-sized sieves, they determined its size, which suggested it was a virus and by subjecting it to various chemicals and determining which ones foiled its ability to infect chimpanzees, they found out that it was surrounded by a lipid envelope. Thus, even before they saw it, isolated it, or knew exactly what it was, scientists had generated information about its physical and chemical structure!!
Alter was also studying NANBH as a disease. Because it tended to produce mild symptoms of liver inflammation, many doctors doubted its clinical significance but Alter showed that about 20 percent of infected people eventually developed cirrhosis, indicating that NANBH was indeed a serious illness. Between 1975 and 1987, NANBH thus began to be recognized as a significant form of hepatitis, and many laboratories joined the efforts to snare the causative agent. Alter had compiled a collection of blood from NANBH patients and chimpanzees, from patients with other liver problems, and from healthy individuals. He organized these into a series of coded samples, for which only he knew the key. Vigorous efforts in dozens of laboratories tried to identify the presumptive virus that caused it but none broke the code.
2. Michael Houghton
Eventually, in 1982, Michael Houghton’s laboratory at the Chiron Corporation, exploited the blossoming methods of molecular biology to isolate the virus, and without any distinctive molecular markers or chemicals to flag the virus, they tracked it down. Rather than stalking the elusive proteins and antibodies associated with the presumptive virus, they aimed instead at the infectious agent’s genetic material. By this time, modern molecular biology techniques were flourishing and included cloning methods to isolate and detect the DNA or RNA that would encode any virus’s machinery. However, because the NANBH germ was so rare, and because no one had uncovered a distinctive molecular tag, the project was similar to searching for a needle in a haystack without the ability to see or feel the needle. Using infected chimpanzee tissue provided by Bradley, the group sorted through tens of millions of pieces of genetic material, looking for a segment that was present in infected, but not uninfected, individuals. Provocative results emerged numerous times, but in each case, the piece of genetic material proved to arise from a source other than the NANBH agent.
In 1985, Houghton and his Chiron colleagues, Qui-Lim Choo and George Kuo, embarked on a risky approach: they attempted to identify DNA or RNA that encoded viral proteins that would bind to antibodies assumed to be present in NANBH-infected chimpanzee and patient sera. This venture represented a scientific fishing expedition in which the researchers weren’t sure they had either fish or bait. As a source of the virus, they used infectious chimpanzee blood and liver — even though they couldn’t directly detect viruses in those samples. For bait, they used blood from chimpanzees and patients infected with NANBH, guessing that it contained antibodies that recognized viral proteins even though no one had evidence for such antibodies. It was unclear if such a ‘blind’ approach would succeed in identifying an infectious agent whose properties were largely unknown. They extracted RNA and DNA from the chimpanzee samples and made DNA copies of it, which they cut into pieces expected to encode parts of proteins, and then they inserted these bits of genetic material into bacteria and forced the bacteria to churn out large amounts of the corresponding proteins. The researchers sought bacteria that produced a protein that bound antibodies from infected, but not uninfected, people, and in a technical tour de force, they screened tens of millions of bacteria in two years. Finally, in one bacterium they hooked their potential quarry.
Next, they had to figure out whether this piece of protein represented the virus they sought, or if it was another false lead. Serum from many different NANBH patients grabbed this protein, while that from uninfected individuals slid off. The DNA that encoded the protein bound to a large RNA molecule in infected material, but not in control tissue and the DNA did not reside in the host’s genome. These results strengthened the hypothesis that the protein they had identified came from the viral culprit, and not from the host. Furthermore, treating the infectious samples with enzymes that destroyed RNA obliterated the positive result, while procedures that destroyed DNA left it intact. This observation indicated that the viral genome was made of RNA. Using the small nucleic acid handle that they had isolated, the researchers plucked out other pieces of the viral RNA. With these, they produced different viral proteins in bacteria and yeast and used them to capture antibodies from humans and chimpanzees infected with NANBH. They detected binding only to blood from NANBH sources, not to blood from individuals infected with hepatitis A or hepatitis B. These findings convinced the researchers that they had achieved their goal. Shortly afterward, they asked Alter to send the panel of samples that had stumped everyone so far, and using their new test, they broke the code! The Chiron team also collected blood from all over the globe and showed that the new virus, which they named hepatitis C virus (HCV), was associated with NANBH worldwide. The researchers could identify most cases of the disease, indicating that HCV was the most common cause of NANBH.
3. Charles Rice
With their new and ambitious virus hunting method, the Chiron team had shown for the first time that it was possible to discover a clinically important agent that had not been grown in the lab, microscopically visualized, or identified by even the most sophisticated serologic technique. The work of Alter and Houghton established a critical link between NANBH and HCV infection. However, it did not constitute definitive proof of causality because transmission of the disease by transfer of infectious blood could not exclude the involvement of essential cofactors. To conclusively demonstrate causality, the isolation of a virus capable of reproducing the clinical hallmarks of the disease, including chronic liver damage and persistence of the infectious virus in the blood of the infected host, was required. A first step towards achieving this goal was made when the groups of Kunitada Shimotohno, working at the National Cancer Center Research Institute in Tokyo, and Charles Rice, then at Washington University in St Louis, in close succession identified a conserved, non-coding region at the 3’ end of the HCV RNA genome, which they surmised could play an important role in virus replication and implied that all of the constructed genomes had failed to replicate in the lab because they lacked this crucial feature. Rice and his postdoc, Alexander Kolykhalov, constructed viral RNA genomes containing the conserved 3’ region, injected them into the liver of chimpanzees, and looked for evidence of HCV replication but failed to observe newly produced viruses in the blood. The ability of the replicons to bestow a survival advantage upon host liver cells had given the researchers a chance to detect HCV replication in the lab but surviving cells contained thousands of RNAs and only about one in a million cells that received the input RNA survived.
Knowing that RNA virus replication is error-prone and that many viral sequences carry inactivating mutations, Rice then took the next decisive step, and engineered a set of RNA genomes that comprised both the conserved 3´ region and a consensus sequence to exclude potential inactivating mutations. He injected the engineered RNA into the liver of chimpanzees and this time the experiment was successful. It turned out that the replicons that had flourished had picked up adaptive sequence changes inside cells and after the investigators engineered these replication-enhancing mutations back into the starting RNA, production of infected cells jumped 500- to 10,000-fold! Productive infection was established, the animals developed clinical signs of hepatitis, and infectious virus was found in their blood for several months. A similarly engineered HCV RNA was soon thereafter reported by the laboratory of Jens Bukh, then at the NIH, also showing that productive infection could be achieved, and for the first time, researchers had generated efficient HCV replication in the lab and because the replicons did not produce infectious virus particles, the system could be used safely without high-level precautions and furthermore, the mini-genomes encoded proteins critical for HCV multiplication, important drug targets. Thus the work of Charles Rice provided conclusive evidence that HCV alone could cause hepatitis, persist long-term, and stimulate a specific antibody response, all features of the human infection.
4. Conclusion
This year’s Nobel Prize is awarded to three exceptional scientists coming from a diverse set of backgrounds whose discovery of the hepatitis C virus and its mechanisms is a landmark achievement in the ongoing battle against viral diseases and is a true example of a bench to bedside discovery for the greatest benefit to humankind! Alter cemented his name at a renowned public research institution, Houghton harks back to a bygone era of outstanding industrial chemists, and Rice is a typical academic scientist who reined supreme at his university research lab. It always made sense to commemorate a virus discovery when another virus is ravaging the world by birthing a global pandemic but not only does today’s prize recognize the power of basic science and virology in the time of Covid-19, but is also a very important step towards destigmatizing hepatitis C. The Hepatitis C virus is a very different virus from SARS-CoV-2. It is easily transmitted by needles, people can be easily reinfected, and mutates at a very high frequency, thereby rendering a vaccine ineffective. The RNA viral pathogen responsible for this severe form of liver inflammation is a leading cause of liver cancer and cirrhosis, afflicting more than 70 million people around the world, and responsible for more than 400,000 deaths annually. The Nobel Laureates have made a decisive contribution to the fight against a major global health problem and a notorious viral disease and thanks to their groundbreaking work, highly sensitive preventative blood tests for the virus are now available and these have essentially eliminated post-transfusion hepatitis in many parts of the world, greatly improving global health. Their discovery also allowed the rapid development of antiviral drugs directed at hepatitis C and for the first time in history, the disease can now be cured, raising hopes of eradicating the hepatitis C virus from the world population, but to achieve this goal, international efforts facilitating blood testing and making antiviral drugs available across the globe will be required along with acknowledging and breaking the inequities that plague the world at large.